How to Improve Patient Experience:
A Complete Guide for Healthcare Leaders
Learn how to improve patient experience by mapping every touchpoint, streamlining operations, and using empathy-driven communication to build patient trust.
TL;DR — Quick Takeaways
- Streamline Processes: Map the entire patient journey to identify pain points that cause friction and frustration.
- Leverage Technology: Use CRMs, patient portals, and automation to reduce manual tasks and improve communication.
- Empower Staff: Free clinical teams from administrative overload through BPO partnerships for scheduling and billing support.
- Train for Empathy: Compassionate, compliant communication builds patient trust and loyalty.
Is your team so buried in administrative tasks that they can’t focus on what truly matters—the patient? If so, you’re not just risking staff burnout; you’re actively damaging the patient experience. Improving it means looking at every single interaction a person has with your organization, from their first call to their final bill, and ensuring communication, efficiency, and empathy are at the core of every step.
Why Patient Experience Is the New Bedside Manner
In today’s world, a patient’s journey is so much more than what happens in the exam room. While clinical skill remains paramount, patients now measure the quality of their care by the entire experience. They’re accustomed to seamless, on-demand service in every other part of their lives, and they bring those same high expectations to healthcare.
This shift puts a spotlight on what used to be considered back-office functions. A confusing phone call to schedule an appointment, a long wait for an insurance pre-authorization, or a bill that makes no sense can completely undermine the trust you’ve built, regardless of how great your medical staff is. The traditional concept of “bedside manner” has expanded to include every single touchpoint, whether digital or in-person.
The True Scope of the Patient Journey
The patient journey is a complex web of moments that, together, shape how people perceive your practice and whether they’ll return. Dropping the ball at any point creates friction that can harm both your reputation and your bottom line. To improve the patient experience, you have to see the whole picture.
- Pre-Visit: This covers everything from a potential patient’s initial Google search and scheduling calls to insurance verification and appointment reminders.
- On-Site: This includes the check-in process, wait times, the consultation itself, and even the cleanliness of your facility.
- Post-Visit: This critical stage covers billing clarity, how payments are handled, follow-up calls or messages, and scheduling their next visit.
Each of these stages is an opportunity to either build confidence or cause frustration. Mastering these operational touchpoints is the essence of modern customer experience management in a healthcare context.
More Than Just Satisfaction
Here’s the bottom line: a positive patient experience leads directly to better health outcomes and a stronger organization. When patients feel safe and supported, they’re far more likely to adhere to their treatment plans and trust their providers.
A recent industry report drove this point home. It showed that patient safety is the bedrock of the entire experience. When patients felt ‘very safe,’ their likelihood to recommend the hospital was a stellar 85.3. But for those who felt even slightly less than safe, that score dropped by over 50 points to just 34.6. You can dig into more of these insights in the Press Ganey ‘Patient experience 2025’ report.
This data proves that running a tight operational ship isn’t just about efficiency. It’s about creating an environment of trust and security that truly defines the modern standard of care.
How to Improve Patient Experience by Mapping Their Journey
Before you can improve the patient experience, you have to see it through their eyes. A patient’s perception isn’t formed during a single visit; it’s built across dozens of small interactions, many of which happen far from the exam room. To truly understand how to improve patient experience, you first need to map out their entire journey.
Mapping this journey means breaking it down into distinct phases and pinpointing the exact moments where frustration can creep in. These “friction points” are often hidden in plain sight—a confusing phone menu, a long wait for insurance verification, or an unclear billing statement. Each one is a chance to either build trust or create doubt.
The Three Core Phases of the Patient Journey
You can think of the patient journey in three main stages. Each presents unique challenges and opportunities for your healthcare practice to shine.
- Pre-Visit: This stage kicks off the moment a potential patient decides they need care. It covers how they find you, the ease of scheduling an appointment, the clarity of the insurance verification process, and any communication they get before their visit.
- On-Site: This is what most people think of as the “care” phase. It includes everything from check-in and wait times to the actual clinical consultation and the check-out process. The physical environment and every staff interaction are critical here.
- Post-Visit: The journey isn’t over when the patient walks out the door. This phase includes billing clarity, payment options, follow-up communication, scheduling future appointments, and managing prescriptions.
This visualization lays out the end-to-end patient journey, from that first phone call to the clinical care and the final bill.
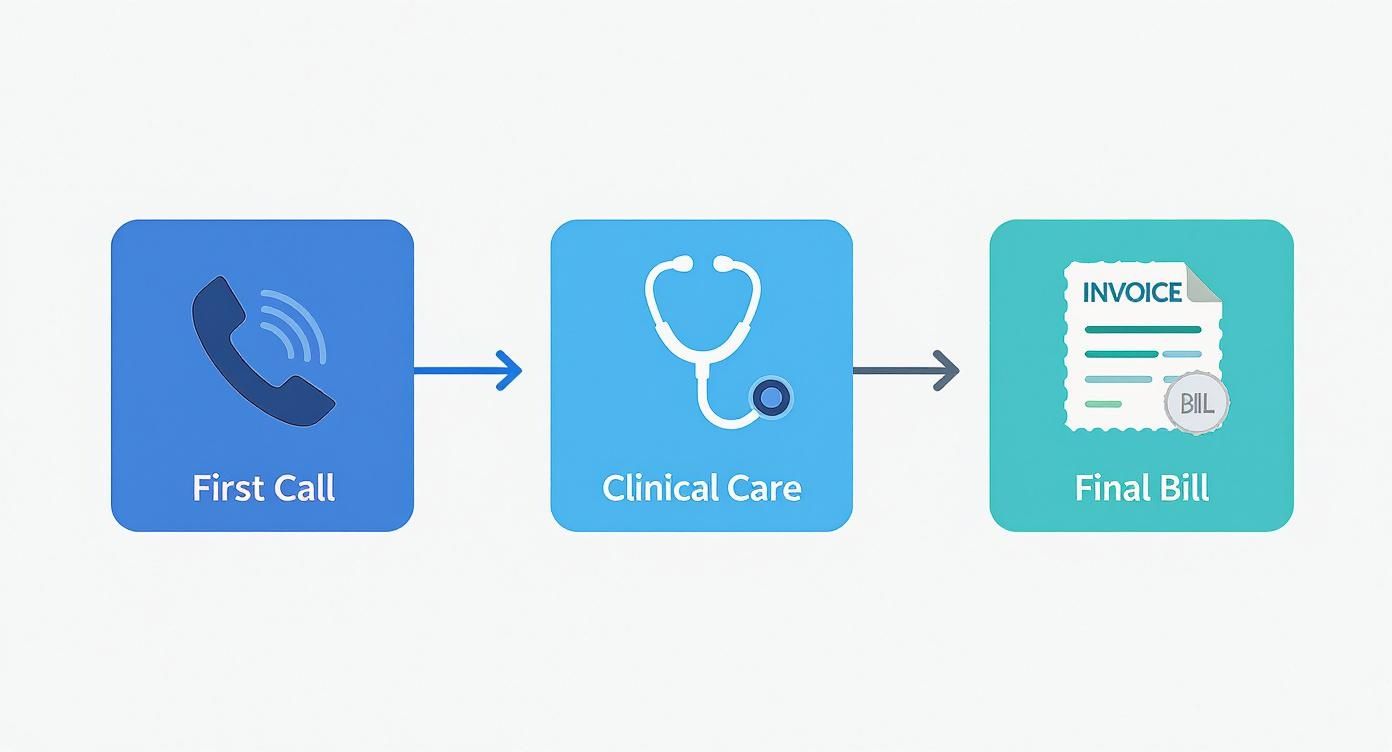
As the graphic shows, administrative touchpoints bookend the entire clinical experience, highlighting just how much impact they have on a patient’s overall perception.
How to Find Hidden Frustrations to Improve the Patient Experience
Once you’ve outlined the stages, dig deeper to find the exact moments that cause stress. For instance, a patient calling to ask a simple question about their bill might have to navigate a complex phone tree, wait on hold for 10 minutes, and then get transferred twice. That single negative interaction can overshadow the excellent clinical care they received.
Similarly, a delay in prior authorization doesn’t just slow down a process; it creates genuine anxiety for a patient waiting for a critical procedure. Research backs this up—consistency is key. A national survey found a strong positive link between outpatient and inpatient satisfaction, proving that patients expect high-quality service at every single touchpoint.
The moments that truly define a patient’s experience often have nothing to do with medicine. They are operational and communication challenges that can be solved with the right strategy and support.
By systematically auditing your own processes, you can pinpoint these friction points. This is where many healthcare providers discover they need specialized support. A nearshore BPO partner, for example, can provide a dedicated team trained in empathetic communication to handle scheduling and billing inquiries, instantly smoothing out two of the most common rough spots. To effectively gauge where you stand, it’s vital to explore different customer satisfaction measurement methods.
The table below breaks down common issues at each stage of the patient journey and shows how a BPO partner can step in to solve them.
Key Patient Journey Touchpoints and Improvement Opportunities
| Journey Stage | Common Patient Pain Point | How a BPO Partner Helps Improve Patient Experience |
|---|---|---|
| Pre-Visit | Difficulty scheduling an appointment; long hold times on the phone. | Provides 24/7 appointment setting services with trained agents, reducing wait times and booking abandonment. |
| Pre-Visit | Confusion over insurance coverage and prior authorizations. | Offers specialized teams for benefits verification and prior authorization management, ensuring clarity for patients. |
| On-Site | Long check-in lines and administrative paperwork delays. | Implements pre-registration calls and digital intake processes to streamline the check-in experience. |
| Post-Visit | Unclear billing statements and complex payment processes. | Deploys trained billing specialists to handle inquiries with empathy and offers clear, simple payment options. |
| Post-Visit | Lack of follow-up communication or appointment reminders. | Manages automated and live follow-up calls, ensuring patients feel cared for even after they’ve left the office. |
By addressing these specific touchpoints, you’re not just fixing small problems; you’re fundamentally improving the patient’s trust in your practice and their overall perception of the care you provide.
Streamlining Operations to Elevate Patient Care
Think of inefficient backend processes as cracks in your clinic’s foundation. You might not see them, but they can destabilize the entire structure. In healthcare, those operational cracks almost always manifest as a poor patient experience. A smooth, empathetic patient journey absolutely depends on a well-oiled machine running behind the scenes.

When administrative tasks bog down your clinical team, patient care suffers. That’s why implementing robust healthcare process improvement strategies is fundamental to boosting both the quality and efficiency of care. This isn’t just an internal goal; it’s a top priority for healthcare leaders everywhere.
In fact, a recent outlook from Deloitte revealed that over 70% of C-suite executives in major developed countries see improving operational efficiency as a key strategy for enhancing the patient experience. The full 2025 global health care executive outlook confirms a critical truth: better operations lead directly to better care.
How Operational Support Directly Boosts Patient Satisfaction
Let’s draw a straight line from specific back-office functions to the front-line patient experience. Optimizing these areas is one of the most effective ways to improve patient satisfaction without adding more pressure on your already stretched medical staff.
- Optimized Appointment Scheduling: Long hold times or a clunky online portal can make patients give up before they even book. A dedicated team ensures every call is answered promptly and professionally, reducing stress from the very first interaction. A practical example is a patient who can schedule a specialist visit in under two minutes via phone, versus waiting on hold for fifteen minutes.
- Demystified Medical Billing: A surprise bill is one of the fastest ways to destroy patient trust. Having trained specialists available to patiently explain charges and payment options can turn a negative experience into a positive one.
- Efficient Prior Authorization: Delays in getting approvals for procedures or medications are more than an inconvenience; they cause real anxiety. A streamlined process ensures patients get the care they need without stressful, unnecessary waiting.
By addressing these core administrative functions, you free up your clinical staff to do what they do best: care for patients. This strategic shift is at the heart of effective business process outsourcing in healthcare, turning operational support into a powerful asset.
Real-World Example: A multi-location urgent care clinic was drowning in billing-related complaints. Their front-desk staff, juggling check-ins and clinical questions, simply couldn’t provide the detailed answers patients needed. After outsourcing their billing inquiry line to a dedicated nearshore team, the clinic saw a 40% reduction in patient complaints within three months and a noticeable spike in positive online reviews mentioning “helpful staff.”
This scenario perfectly illustrates the core principle. When you lift the administrative burden from your clinical team, you empower them to deliver higher-quality, more focused, and more empathetic patient care.
Using Technology to Create a Connected Experience
Technology can be a game-changer for the patient experience, but only when it supports the human connection—not replaces it. The right tools should make healthcare more convenient and less confusing, creating a seamless journey that still feels personal and supportive.
The goal isn’t just to digitize old processes; it’s to build a truly connected experience. Think of it as building a digital front door that’s always open but has a friendly guide ready to help the moment someone gets stuck. For many healthcare providers, a practical guide like this Ewait setup implementation guide for clinics can offer actionable steps to get started.
Building a Single Source of Truth
One of the biggest frustrations for patients is repeating their story over and over to different people. A robust Customer Relationship Management (CRM) system solves this by acting as a single source of truth, centralizing every interaction a patient has with your practice.
When an agent answers the phone, they should see a complete history: past appointments, billing questions, and notes from previous conversations. This allows them to provide context-aware support that makes the patient feel heard and understood, eliminating the dreaded, “Let me transfer you… you’ll have to explain it all again.”
Empowering Patients with Self-Service Options
Modern patients expect modern convenience. A well-designed patient portal is an essential tool for giving them control over their healthcare journey.
- Appointment Management: Patients can book, reschedule, or cancel appointments online without making a call.
- Access to Information: They can view lab results, read visit summaries, and access educational materials 24/7.
- Secure Messaging: Portals provide a secure, HIPAA-compliant channel for asking non-urgent questions, ending the cycle of phone tag.
But technology alone is never enough. The moment a patient struggles to log in or can’t find what they need, a human touch becomes critical. This is where a BPO partner provides an essential support layer, offering live agent assistance to resolve portal issues in real-time.
The best technology empowers patients but also provides an immediate, human-powered escape route when self-service fails. A friendly voice ready to help turns a moment of tech frustration into a positive, brand-affirming interaction.
This balanced approach ensures you get the efficiency of automation without sacrificing the compassionate support that defines excellent healthcare. Integrating the right medical practice management software is fundamental to creating this cohesive, tech-enabled ecosystem.
The Power of Empathy in Healthcare Communication
Clinical skill is essential, but that expertise can be undone by a single cold, impersonal phone call. The most advanced medical care feels hollow if the human interactions surrounding it lack warmth and understanding.
Empathy isn’t just a “nice-to-have” soft skill. It’s a non-negotiable part of every patient interaction, from a routine scheduling call to a sensitive billing discussion.

This is especially true when patients are at their most vulnerable. Someone calling about a confusing bill isn’t just asking about numbers; they’re often worried about their finances. A caller trying to reschedule a critical appointment might be juggling work, family, and anxiety. An agent who only hears the request without recognizing the emotion behind it has already failed the patient.
Training for Compassion and Compliance
Effective healthcare communication demands specialized training that goes beyond a standard customer service script. Agents must become experts in both compassion and compliance—a delicate balance that is critical for building trust and protecting your practice.
This is where a dedicated BPO partner proves its worth. We don’t just hire for technical skills; we hire for innate empathy. Then, we invest heavily in rigorous, healthcare-specific training that covers:
- Active Listening Techniques: Teaching agents to hear the unspoken concerns in a caller’s voice, allowing them to respond to the emotion, not just the words.
- De-escalation Strategies: Equipping teams with the tools to calmly and effectively manage conversations with distressed or frustrated patients.
- HIPAA Compliance: Ensuring every interaction, no matter how empathetic, strictly adheres to patient privacy regulations to maintain professionalism and trust.
Understanding this deep connection between compassion and loyalty is core to our approach. That’s why we’ve dug deep into the role of empathy in customer service as a fundamental business strategy.
Empathy in Action: A Tale of Two Calls
Let’s walk through a real-world scenario. A patient, anxious about an upcoming procedure, calls because their pre-authorization hasn’t been approved yet.
- The Poor Response: “I see it’s still pending in the system. You’ll have to wait for the insurance company to process it. I don’t have any other information for you.” This response is factually correct but completely dismisses the patient’s anxiety, leaving them feeling helpless and unheard.
- The Empathetic Response: “I can see how stressful it is to be waiting on this, especially with your procedure coming up. Let me confirm we have all the correct information submitted from our end. I’m also going to set a reminder to check the status for you tomorrow morning and give you a quick call back with an update, even if nothing has changed.”
The difference is profound. The first agent closed a ticket; the second agent built a relationship. The empathetic approach validates the patient’s feelings, offers proactive help, and provides reassurance, turning a moment of friction into an opportunity to strengthen trust. This is how you improve the patient experience, one compassionate conversation at a time.
Answering Your Patient Experience Questions
As healthcare leaders begin to analyze the patient journey from end to end, several key questions consistently arise. Moving from a high-level strategy to on-the-ground implementation requires clear answers about resources, reputation, and return on investment.
Here are some of the most common questions we hear from clinics and hospitals ready to make a change.
What Is the First Step to Improve Patient Experience?
Before you invest in new technology or overhaul processes, the most impactful first step is to map the entire patient journey. See your practice through your patients’ eyes.
Trace every touchpoint, from their initial Google search to their post-visit follow-up call. More importantly, solicit feedback to identify the biggest friction points. Is scheduling an appointment a nightmare? Are your billing statements confusing? Zeroing in on the most significant pain point first will deliver the biggest win and build momentum for further improvements.
 How Can We Measure the ROI of Improving Patient Experience?
How Can We Measure the ROI of Improving Patient Experience?
Measuring the return on investment for patient experience initiatives requires tracking both patient-centric and hard financial metrics. A superior experience has a direct, measurable impact on your bottom line.
Start tracking these key performance indicators:
- Patient Retention Rates: Happy patients are loyal patients. A reduction in patient churn is a direct financial gain.
- Online Review Scores: Monitor ratings on sites like Google and Healthgrades. Better scores act as a magnet for new patients.
- Faster Payment Collection: When the billing process is clear and the support team is helpful, patients are more likely to pay their bills on time.
- Patient Satisfaction Surveys: Use tools like the Net Promoter Score (NPS) to gauge patient loyalty and their likelihood to refer others.
Is Outsourcing Patient Communication Risky?
That’s a valid concern. The risk isn’t in outsourcing itself—it’s in choosing the wrong partner. A generic call center could be a risk to your reputation. A specialized healthcare BPO, however, is designed to mitigate that risk.
A quality partner acts as a seamless extension of your team, not just a call handler. They invest heavily in industry-specific training, rigorous HIPAA compliance, and empathy-focused coaching to ensure they are guardians of your patient relationships.
The key is to find a partner who understands the nuances of healthcare and is committed to embodying your brand’s voice and professional standards in every conversation.
Where Can a BPO Help Our Burned-Out Staff Most?
If your clinical staff is drowning in administrative tasks, a BPO can be a lifeline by immediately taking over high-volume, non-clinical work. This frees up your skilled team to focus on what they do best: patient care.
We see the biggest and fastest impact in these areas:
- Appointment scheduling and reminders
- Insurance verification and prior authorizations
- Handling first-level billing questions and payment support
Taking these tasks off your team’s plate can slash burnout and instantly improve the quality of every patient interaction in your facility.
🚀 Ready to Elevate Every Patient Interaction?
CallZent provides empathetic, compliant communication and back-office solutions that help your healthcare team focus on what truly matters—delivering exceptional care.
Ready to elevate every patient interaction without overwhelming your team? CallZent provides specialized, empathetic communication and back-office solutions that allow you to focus on what matters most—delivering exceptional care. Discover how our nearshore support can transform your patient experience by visiting us at https://callzent.com.


 How Can We Measure the ROI of Improving Patient Experience?
How Can We Measure the ROI of Improving Patient Experience?







